STEM CELL PREPARATION
When it is decided to use stem cells, the stem cells are procured either from the bone marrow or the fat from the hip region. In human and veterinary medicine, it is unclear whether bone marrow or fat derived stem cells are more advantageous, but we know that both tissue yield high levels of stem cells. At CEC, we prefer to harvest stem cells from the bone marrow because we can keep these cells in their same environment, concentrate them, and while they are still in their “home” environment, inject them within two hours into the damaged tissue.
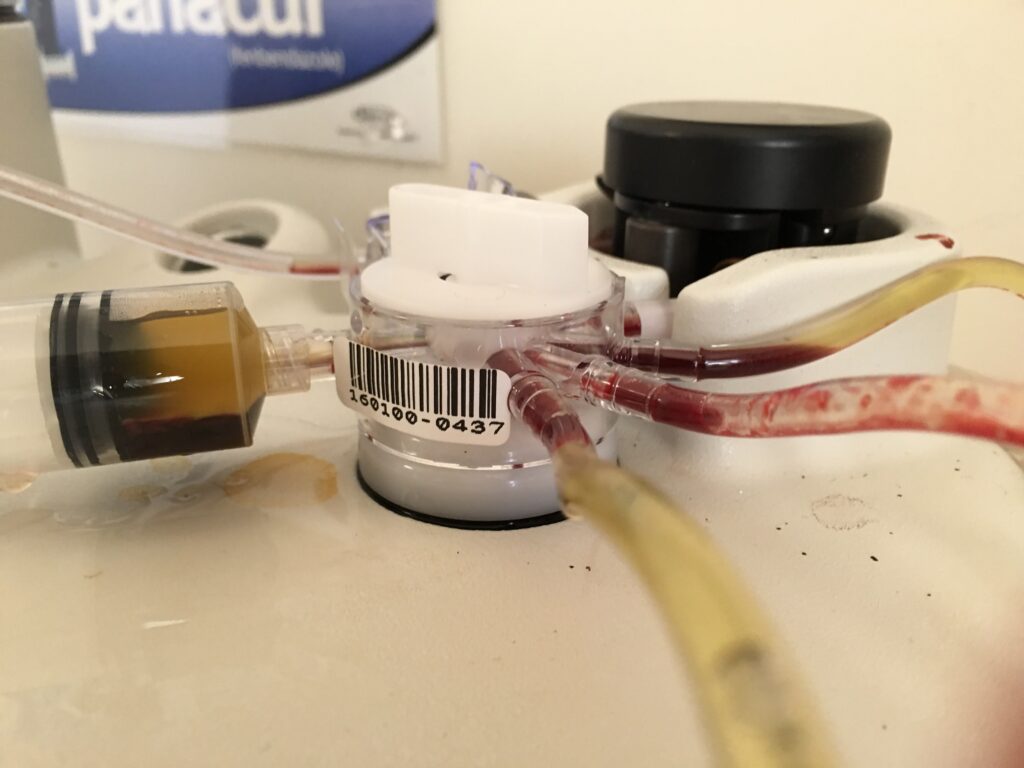
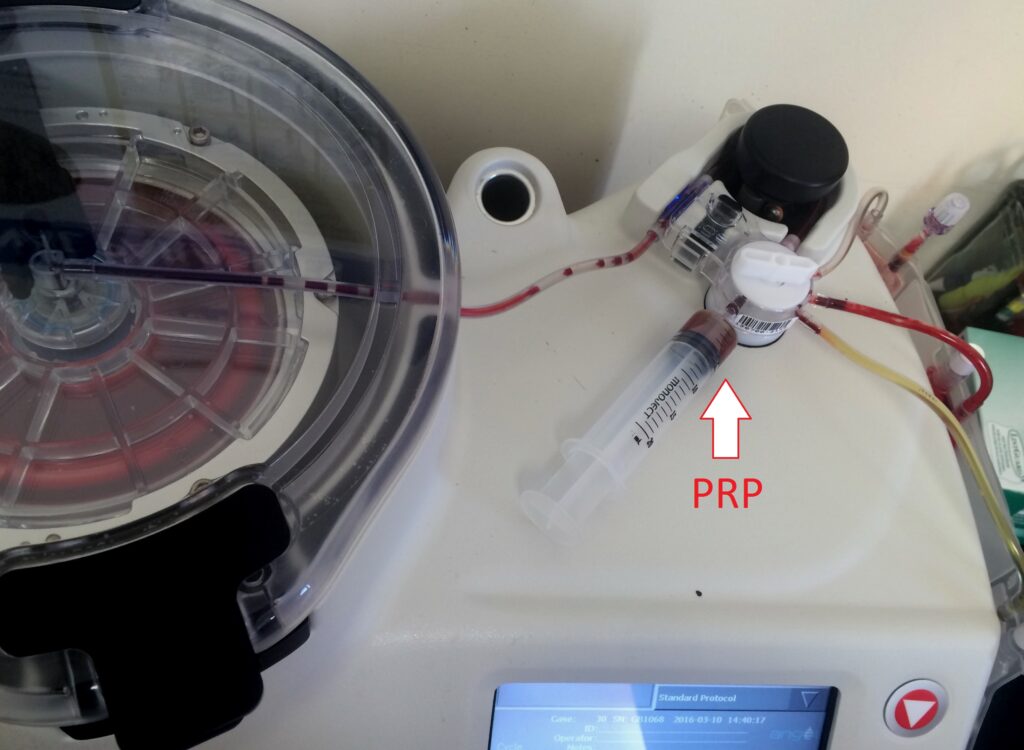
The process is after identification of the body and tissue depth of a sternal bone using ultrasound, sterile preparation and local anesthesia of the tissue. A large bore needle with a marked stylet is used to bore into the bone. Next, 2 – 3cc of heparin is injected into the bone as bone marrow clots very fast, and then 60cc of bone marrow is removed. The location is bandaged, and the 60cc of bone marrow stem cell is centrifuged. As in preparation of platelet rich plasma, stem cells have a specific weight and thus can be concentrated with centrifugation by special equipment.
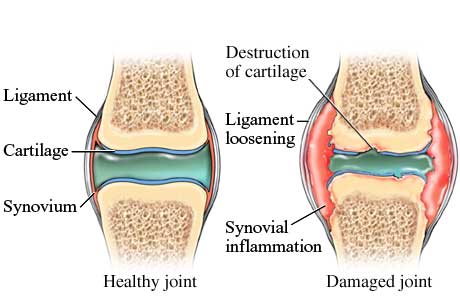
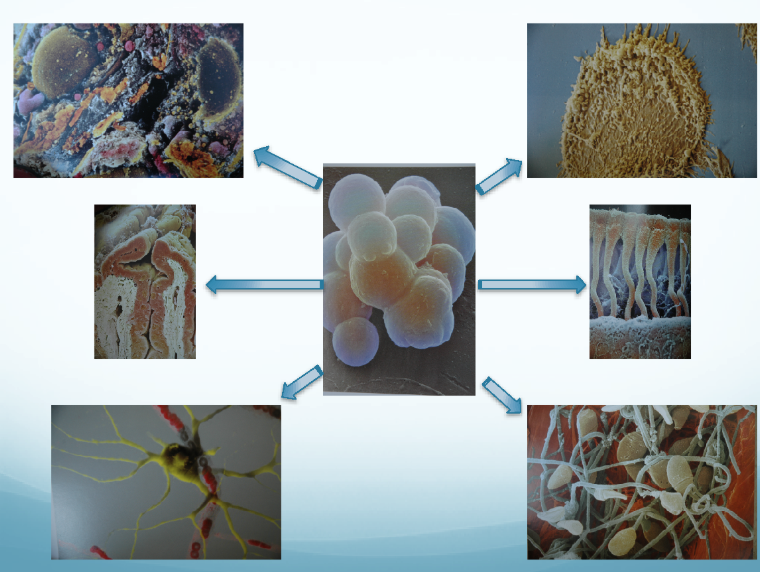
These cells are then injected into the joint or tendon, or even used as a regional limb perfusion. Stem cells can “hone” which means they migrate to the area where they are needed, and differentiate into the cell type needed in that area. Some clinicians send stem cells to labs to grow the stem cells into larger numbers before injecting. It is yet unknown how many stem cells are needed to produce the desired effect.
FACTORS FOR SUCCESS FOR ORTHOBIOLOGIC TREATMENTS
As in any treatment of the musculoskeletal system, several factors are involved to achieve the optimal success:
- An accurate diagnosis to include examination of the whole horse
- Preparation of the PRP using advanced centrifuges
- Injection using sterile technique and ultrasound guidance to assure accurate location of PRP
- Physical therapy post injection
- Recognition and treatment of mechanical interferences
CONTRAINDICATIONS
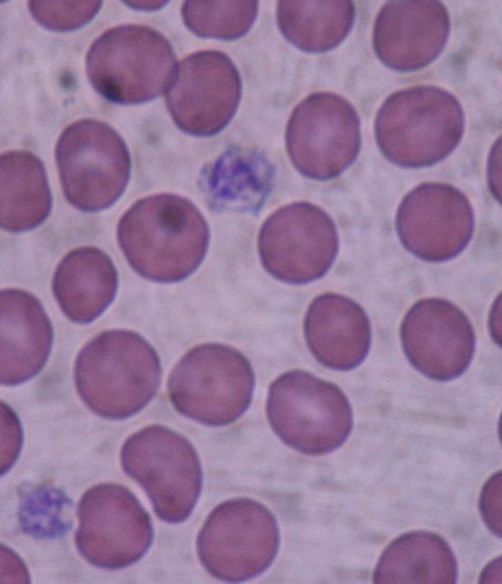
The use of biologics is contraindicated in horses that are septicemic (have a systemic infection), have received corticosteroid injections at the same site within the past two weeks, have recently been feverish or ill, or have a low systemic platelet count. The risk of worsened pain or reduced function is very low in both humans and horses—significantly lower than the risks associated with corticosteroid joint injections. While temporary pain at the injection site may occur, it is rare. For PRP to be effective, it must be injected directly into the lesion; otherwise, it will not have the desired effect. Ultrasound-guided injections are crucial to ensure PRP is accurately deposited into the damaged tissue rather than surrounding healthy tissue. The risk of infection is extremely low.
SUMMARY
In summary, regenerative medicine may represent the future of medical treatment. Why not harness the body’s natural ability to activate cell activity and produce new cells using the animal’s own biological resources? By creating the right environment for these active progenitor cells to function, we provide both the conditions and the tools for healing. This concept is similar to providing a plant seed with water, warmth, nutrients, and soil to grow.
In severe cases of osteochondrosis dissecans, the combination of PRP and stem cells has shown better outcomes than surgery, injectable medications like Adequan or hyaluronic acid, or steroids. Since 2008, Colorado Equine Clinic has treated over 345 cases, addressing more than 850 areas, including tendons, joints, hoof cracks, laminitis, and draining fistula tracts, using PRP with or without stem cells. The results have been longer-lasting, with shorter recovery times and significant pain reduction lasting several years. In some cases, horses have required no further treatment for years.
However, each case is unique, and client needs and goals vary. We are grateful to have access to these regenerative therapies, especially given the superior clinical outcomes we’ve observed. These results reinforce the value of considering orthobiologics as a viable option for treating musculoskeletal injuries in horses.